What the heck is that psych med for?? How do SSRIs and other psychiatric medications work? bridge provides digestible medication information and an interactive therapist resource for what psychiatric medications treat and the theory behind each major class of medications. Because who has time to go to medical school?
The table below provides an interactive list of psychiatric medications. Below that table is a brief and simple description of the theory behind common classes of medications (e.g., SSRI, SNRIs, mood stabilizers, antipsychotics, and more) and a brief list of common negative medication interactions. The table allows you to scroll from side-to-side when viewing on mobile.
There is also a good book that provides easy reference on psychiatric medications by disorder and another good book on medications that is highly simplified. Another good book provides easy reference on psychiatric medications for children and adolescents.
Any links in the table below to pharmaceutical website pages are used for informational purposes and are not affiliate- or partnership-based (we do not receive money for directing you to those web pages).
Table of Psychiatric Medications
To change the order of how to view medications in the table below (for instance, alphabetically by name, by what it treats, or by class), hover your mouse on the right side of the top line of each column and click the small arrows. Click the class / mechanism of action of each medication to go to a description of the theory behind that class of medication.
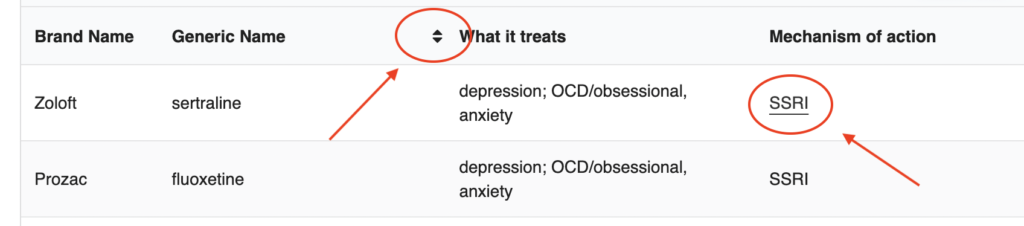
You can search for specific medications, what a medication treats, or classes of medications in the Search field at the top of the table. You can also hit “Control” and hold “F” (“Command” and hold “F” for Mac) to get a search bar that allows for any term on the page to be searched directly (this can be done on almost any Internet page).
Classes of Psychiatric Medications
Anti-anxiety
Also referred to as “anxiolytics”, anti-anxiety medications have a few different mechanisms of action. Some anxiolytics directly affect neurotransmitters related to anxiety (e.g., benzodiazepines). However, others may have been created for other primary purposes but appear to have some beneficial effects related to anxiety (e.g., beta-blockers; antihistamines like hydroxyzine).

Benzodiazepines
Benzodiazepines work on gamma-aminobutyric acid (GABA). GABA is an amino acid that inhibits or slows the excitability of messages transmitted between brain cells, creating a calming effect in the brain. Benzodiazepines increase how effectively GABA functions when it is transmitting from one brain cell to the next. This reduces excitability of brain cells throughout the brain and create a greater calming effect for the individual. Additional applications include the treatment of insomnia. Benzodiazepines tend to be highly addictive and have a number of dangerous interactions with other classes of medications (e.g., opiate pain medications).
Examples: Xanax (alprazolam), Valium (diazepam), Ativan (lorzepam), Klonopin (clonazepam)
Other anti-anxiety medications
There are multiple other non-benzodiazepine anxiolytic medications. A commonly used anxiolytic is the antihypertensive class called beta blockers. Beta blockers “block” the hormones adrenaline and noradrenaline from binding to cells in the heart and to parts of the sympathetic nervous system (the system associated with “fight or flight”). This process blocks increases in heart rate in order to relieve many of the physical symptoms of anxiety (e.g., rapid heartbeat, trembling, sweating, etc). Beta blockers can decrease the chance of panic attack, but they can also disturb sleep. The USDA does not formally recognize these as an anxiety treatment.
Examples: Indero (propranolol), Tenormin (atenolol)
Other anxiolytics include barbiturates, which have a similar effect as benzodiazepines. However, they have a much higher risk for overdose (so they are not used as much for anxiety). Some also have anticonvulsant effects.
Examples: Nembutal (pentobarbital), Lumina (phenobarbital), Mysoline (primidone)
Azapirones are another class of anxiolytic medication. Azapirones promote activity of serotonin in some parts of the brain cell, but inhibit serotonin in other parts. Buspirone (aka Buspar) is the most common medication in this class. Buspirone increases transmission of serotonin throughout cells while providing mild decreases in dopamine transmission. prescribers also use this to depression and some neurological conditions (e.g, Parkinson’s, some dementias, and behavioral difficulties following TBI). It can also increase the effectiveness of some antipsychotic treatments.

Antidepressants
Antidepressants have a number of mechanisms of action to aid transmission of biochemicals between brain cells. These include effects on serotonin, norepinephrine, and dopamine at different levels or combinations of these neurotransmitters.
SSRIs – Selective serotonin reuptake inhibitors
Serotonin has effects on mood, sleep, and sexual desire, among other functions. SSRIs fight depression by allowing more existing serotonin to sit between brain cells for longer. This allows a greater chance of neighboring brain cells catching serotonin and further transmitting it through the brain (they do not produce new serotonin). SSRIs have also shown benefit for anxiety and obsessional processes in conditions like OCD or OCPD.
Examples: Prozac (fluoxetine), Zoloft (sertraline), Paxil (paroxetine)
SNRIs – Serotonin-norepinephrine reuptake inhibitors
Norepinephrine (a.k.a. “noradrenaline”) is linked to arousal, alertness, and attention. SNRIs fight depression by allowing more existing serotonin and norepinephrine to sit between brain cells to increase the chance neurotransmitters will catch them and pass them around the cells (they do not produce new serotonin or norepinephrine). SNRIs have also shown benefit for anxiety and chronic pain.
Examples: Effexor (venlafaxine), Cymbalta (duloxetine), Pristiq (desvenlafaxine)
NDRIs – Norepinephrine and dopamine reuptake inhibitors
Dopamine is associated with reward, motivation, attention, and arousal (among many other functions). DNRIs fight depression by allowing more existing norepinephrine and dopamine to sit between brain cells to increase the chance neurotransmitters will catch them and pass them around the cells (they do not produce new norepinephrine or dopamine). NDRIs have also shown benefit for anxiety, bipolar disorders, and ADHD.
Example: Wellbutrin (bupropion); methylphenidate (e.g., Ritalin) is suspected to be in this class
Tricyclic antidepressants (TCAs)
Tricyclics are similar to SNRIs. They work by allowing more existing serotonin and norepinephrine to sit between brain cells, allowing more existing serotonin and norepinephrine to sit between brain cells to increase the chance neurotransmitters will catch them and pass them around the cells . However, they are older medications with more negative side effects. Due to this, prescribers usually attempt to use newer antidepressants like SSRIs or SNRIs. Prescribers sometimes use Tricyclics when those other medications do not show benefit. Tricyclics can also treat migraines, neuropathic pain, and insomnia.
Examples: Tofranil (imipramine), Pamelor (notriptyline), amitriptyline
MAOIs – Monoamine Oxidase Inhibitors
MAOIs inhibit or slow the breakdown of serotonin, norepinephrine, and dopamine (these are sometimes referred to as “monoamine neurotransmitters”) to allow them to be more available in the brain and gut. These medications were the first antidepressants to receive approval. They have more negative side effects than newer antidepressants like SSRIs or SNRIs. Despite this, prescribers often use it if other antidepressants are not effective.
Examples: Nardil (phenelzine), Parnate (tranylcypromine)
Antipsychotics
Antipsychotics act as “dopamine antagonists”. The dopamine hypothesis posits that high levels of dopamine passing between brain cells accounts for many symptoms of schizophrenia (especially positive symptoms like hallucinations and delusions). Antipsychotic dopamine antagonists “antagonize” or reduce the amount of dopamine available to pass between brain cells in order to limit those symptoms. There are 2 main types of antipsychotic meds.

Atypical antipsychotics (2nd generation)
Atypical antipsychotics inhibit dopamine transmission but also have affects on serotonin. They are thought to have less severe long-term side effects and can impact negative symptoms in addition to positive symptoms.
Examples: Risperdol (risperidone), Seroquel (quetiapine), Clozaril (clozepine), aripiprazole (Abilify)
Typical antipsychotics (1st generation)
Typical antipsychotics mainly inhibit dopamine. Although they have more side effects and mostly relieve positive symptoms, they may not be effective for all patients. Some patients may respond better to these medications, so they are still widely used.
Examples: Haldol (haloperidol), Prolixin (fluphenazine), Thorazine (chlorpromazine)

Mood Stabilizers
Mood stabilizers intend to decrease frequency and magnitude of extreme fluctuations between states of (hypo)mania and depressive episodes seen in bipolar disorder. Examples of mood stabilizers include lithium and certain anticonvulsants.
Lithium salts (aka “lithium”)
The way lithium works is not fully understood. However, it is thought to break down certain enzymes to prevent them from being recycled and used again by brain cells. During mania, lithium appears to protect cells from succumbing to metabolic stress and to prevent the release of neurotransmitters (especially dopamine and serotonin). This protective process slows or stabilizes how those chemicals transmit around brain cells. Lithium has similar properties to sodium (table salt) that allow it to travel far and wide throughout the body and nervous system. This allows lithium to effectively interact with many biological processes throughout the body that culminates in its therapeutic effects.
Anticonvulsants
Anticonvulsants are typically prescribed for seizure disorders like epilepsy. But they have also shown promise for treating bipolar disorders. Brain cells pass messages to each other with the help of electrical impulses. Sometimes those impulses travel too quickly across brain cells, forming an elevated or “excitatory” response. Anticonvulsants tend to help manage transmission of chemicals like glutamate (the brain’s “ON” signal) and GABA (the brain’s “OFF” signal). This management improvement helps create a more “inhibitory” response to slow down those rapid electrical impulses and the passage of messages throughout the brain. This process is thought to also slow down brain cell activity related to mood.
Examples: Valproic (sodium valproate or valproic acid), Tegretol (carbamazepine), Lamictal (lamotrigine)
Stimulants
Current research suggests that lower than average levels of dopamine and norepinephrine play a role in attentional difficulties and hyperactivity. Stimulant medications work with dopamine and norepinephrine in different ways help improve attention, focus, and task completion for those with ADHD. Some stimulant medications are in the amphetamine class. However, anyone taking these medications will note improvements in attention and levels of hyperactivity, so such benefits do not confirm a diagnosis of ADHD.

Reuptake inhibitors
Stimulant medications like Ritalin (methylphenidate) allow more existing dopamine and norepinephrine to sit between brain cells to increase the chance cells will catch it and pass it around the cells. Strattera (atomoxetine) is a nonstimulant medication that allows more existing norepinephrine to sit between brain cells to increase the chance cells will catch it and pass it around parts of the brain. This mechanism tends to improve alertness, attention, and memory.
Increased release medications
Other stimulants like Adderall (amphetamine) promote greater release of dopamine and norepinephrine from storage areas in brain cells. It’s like overfilling a water balloon to get plenty of water all over your target. More dopamine and norepinephrine is available to pass between brain cells and throughout parts of the brain.

Sleep medications
Prescribers often use sedatives for insomnia. These include benzodiazepines or barbiturates, but a “miscellaneous” class includes more modern sedatives. These newer sleep medications mainly increase the transmission of GABA in order to reduce excitability of brain cells and create a slowing or calming effect. However, many of them do not have anticonvulsant or muscle relaxant properties. Additionally, prescribers sometimes use the antidepressant trazodone to treat insomnia.
Examples: Ambien (zolpidem), Lunesta (eszopiclone), Sonata (zaleplon)
Other sleep aids
Melatonin and ramelteon work on melatonin receptors in the suprachiasmatic nucleus in the hypothalamus area of the brain. Those receptors have sleep promoting actions and regulate our sleep/wake cycle. The mechanism of action of melatonin and ramelteon is unique in comparison to other sedatives. They also do not cause withdrawal or physical dependence. Some experts believe melatonin may disrupt sleep/wake rhythms after extensive use. However, a more clear understanding of melatonin’s effects requires more evidence.
As an informational aside, a highly effective nonmedication approach to insomnia is cognitive behavioral therapy for insomnia (CBTi). Developed by researchers at Harvard Medical School, multiple medical organizations have recognized it as the frontline treatment for insomnia, instead of medications. This good book on CBTi by its developer explains the underlying idea. There is also a good video explanation of the theory and some techniques clinicians or clients can use for a quick rundown. This workbook for sleep is based on CBTi and can be used with clients who have trouble sleeping.
Other psych medications
There are a range of other types of less common psych medications. See our medication look-up table resource above for less commonly seen types of medications not listed in these explanations. Links to additional information are provided there.


Negative Interactions
There are many negative interactions between different psych meds and between psych meds and other types of medications. This list does not include all of them. We include examples of negative medication interactions commonly seen in mental health practice and related fields.
Common negative interactions:
- benzodiazepines and opiate pain medications
- benzodiazepines and grapefruit juice
- benzodiazepines and alcohol
- benzodiazepines and thiazolidinediones
- benzodiazepines and some antidepressants
- tricyclic antidepressants and SSRIs
- typical antipsychotics and SSRIs
- atypical antipsychotics and SSRIs
- antipsychotics and alcohol
- narcotics/opioids and alcohol
- SSRIs and MAOIs
- SSRIs and triptans (treat migraines)
- lithium and ACE inhibitors